Prostate cancer is one of the most common cancer types in men. With bone as a frequent metastatic site, response assessments for prostate cancer have additional considerations beyond RECIST 1.1. In our recent webinar, MERIT outlined the fundamentals of the Prostate Cancer Working Group 3 (PCWG3) response criteria, data collection, and response assessment as well as imaging using bone and PSMA PET/CT scans in prostate cancer.
This article focuses on the bone scan and PSMA PET/CT imaging portion of the webinar. Matthew Hoover is MERIT’s Oncology Partnerships Executive and presented the nuclear medicine imaging portion of the webinar. Matt holds an MBA and has an undergraduate degree in Nuclear Medicine Technology, with certifications in Nuclear Medicine, Computed Tomography (CT), and Positron Emission Tomography (PET) through the Nuclear Medicine Technology Certification Board (NMTCB).
Click here to see the full webinar
Scintigraphy: Nuclear Medicine Bone Scan
A bone scan (skeletal scintigraphy) is a special type of nuclear medicine procedure that uses small amounts of radioactive material to diagnose and assess the severity of a variety of bone diseases and conditions, including fractures, infection, and cancer. As mentioned above, bone is a frequent metastatic site for prostate cancer, so bone scans can be a common imaging modality in the disease.
Procedure Overview:
There are no contraindications for performing bone scintigraphy. Patients are free to continue taking their standard medication and can eat and drink prior to their appointment. The imaging procedure itself is straightforward and the entire exam generally takes around 3-4 hours to complete – the actual imaging portion of the exam is usually 30-60 minutes, depending on protocol and if additional views are required.
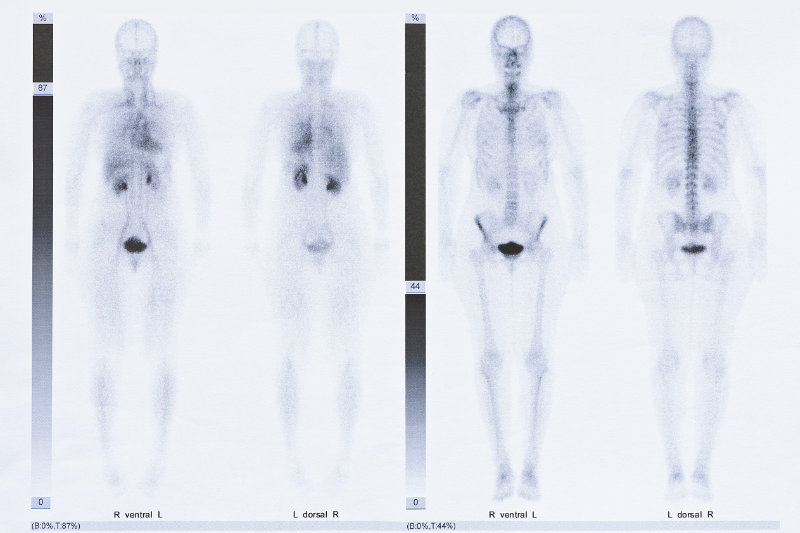
The exam starts with a general patient assessment, noting any recent trauma or injuries (to include biopsies), as well as bone pain. Once that is completed, the technologist will administer the radiotracer intravenously. There are a few different options for radiotracers; however, the two most used imaging agents are:
- 99Technetium methyl diphosphonate, or 99Tc MDP
- 99Technetium hydroxy diphosphonate, or 99Tc HDP
Once administered, both radiopharmaceuticals are taken from the blood stream by the osteoblasts, the cells responsible for bone building, and incorporated into the hydroxyapatite crystal matrix within the bone structure.
For radiopharmaceutical localization, it generally takes 2 to 3 hours post injection for the tracer to work its way from the blood stream and to be incorporated into the bone structure. During the 2–3-hour uptake period, it is important for the patient to increase their fluid intake and void prior to imaging to minimize background radioactivity or noise within the image, to ensure a high target-to-background visualization.
Typically, a whole body, planar image is acquired. Additionally, common optional imaging maneuvers may include:
- Lateral or oblique imaging of an area of concern
- SPECT or SPECT/CT image of a region of interest
- Produces a 3D image of the bone structure versus a 2D image.
Tips for Success
It is important to note that not all “hot spots” are malignancies. Other common reasons for increased uptake or visualization of a hot spot on the images include:
- Recent trauma, such as a fall, bone biopsy, or fracture
- Epiphyseal plate visualization
- Arthritic joints
In addition to ensuring that the patient history is completed in a thorough manner, it is equally important for the local imaging site to:
- Take a series of dedicated pelvic images immediately post void if the bladder is visualized (as is common)
- Ensure that any potential osseous pelvic lesions are visualized versus being obscured by bladder activity
- Carefully follow the study protocol to ensure optimal imaging results
It should be noted that there is a wide dosing range for the radiopharmaceutical. While 30mCi may be appropriate for a gamma camera that is 30 years old (which there are many out there, that still take high quality images), it may be too much activity for a newer, solid-state gamma camera. Newer cameras can utilize a dose that is 15mCi or lower. Details such as this must be addressed within the imaging charter and site manuals to ensure study data is based off optimal imaging parameters.
PSMA PET/CT Imaging
As the name indicates, PET/CT scans combine a CT scan with a PET scan, another type of nuclear imaging test that requires patients to receive intravenous injections of a radioactive “tracer” that can be detected on the scan. In a PSMA PET/CT, the tracer used for the PET scan includes a molecule that specifically binds to the PSMA protein, which is often found in large amounts on prostate cancer cells. That molecule is linked to a radioactive compound, or radioisotope.
Currently, there are many different variations of PET/CT PSMA radiopharmaceuticals in various stages of development and commercial availability, which utilize many different isotopes with varying properties. However, for the majority of the available PET/CT PSMA radiopharmaceuticals today, the isotopes being evaluated or used are 68Gallium or 18Fluorine. Regardless of which isotope is being used, the mechanism of localization is still straightforward for most PSMA PET/CT imaging agents. The imaging agent is removed from the blood stream after administration and binds to the PSMA proteins on the surface of the prostate cancer cells. While localized, the imaging agent emits radiation which is detected by the PET imaging system and then used to create an image, identifying concentrations of the radiotracer throughout the patient.
Procedure Overview:
To perform PSMA PET/CT imaging, there are no contraindications. Patients are free to continue taking their standard medications and can eat and drink prior to the appointment. The imaging procedures itself is straightforward and patients should allow 2-4 hours to complete. In a nutshell, the patient arrives and completes a medical history and medication reconciliation with the technologist performing the exam. An IV catheter is placed, and the radiopharmaceutical is administered. Most facilities will allow the imaging tracer to circulate for around 50 minutes, then ask the patient to void in the restroom, and aim to be imaging the patient at around the 60-minute post-injection mark. Imaging typically is performed 50 to 100 minutes post injection, but high-quality images have been captured even up to the 3-4-hour post-injection time point. The imaging procedure itself typically lasts around 30 minutes and the technologist should begin imaging at the pelvic region and work their way up to the patient’s head, to maximize visibility around the bladder area.
In the example images shown here, all three patient images are positive for PSMA avid regions of interest, indicated by the arrows.
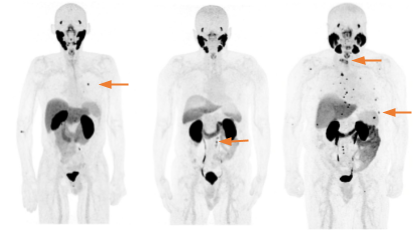
Image Source: Society of Nuclear Medicine and Molecular Imaging
In general, the varying PSMA compounds are very good, being able to image roughly 95% of patients with prostate cancer with accuracy – however, some studies have shown that there is a small population, around 5% of the prostate cancer patients, whose scan may produce a false-negative result due to the lack of or minimal amount of PSMA protein receptors on the cellular surface.
Tips for Success:
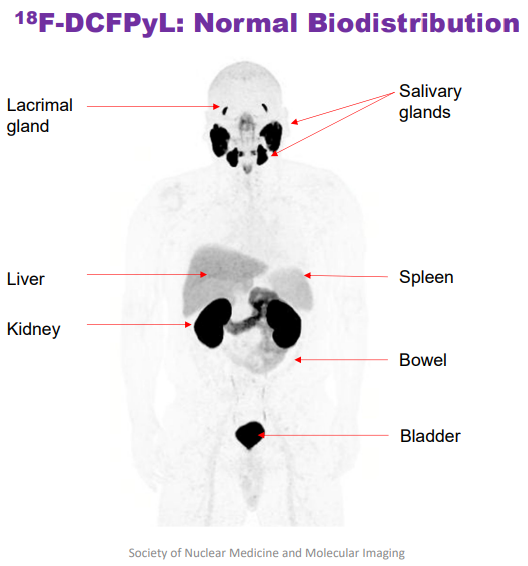
As mentioned earlier, it is important to note that “hot spots” don’t always equate to malignancies. Certain body habitus will consistently show varying degrees of uptake, which is not indicative of a malignancy, but rather is a common and completely normal biodistribution of the radiotracer. While each imaging compound varies slightly and requires specific reader training, the image shown here gives a sense of what areas of the body are commonly visualized which are pathologically unremarkable. For the particular compound shown here, 18Fluorine DCFPyL, it is normal and not alarming to see intense focal uptake in the lacrimal and salivary glands, liver, spleen, kidneys, bowel, and bladder. Factors like normal biodistribution should be considered when performing PSMA PET/CT imaging or any other nuclear medicine study. Reader selection and appropriate training for the particular protocol being used is key for trial success.
In addition to identifying soft tissue mets, the PSMA agents in development are fairly good at identifying bone metastasis. However, more information is needed in this area, which is why the standard is to still to include some form of functional bone imaging such as a 99Tc-MDP bone scan or even a sodium 18fluoride PET bone scan.
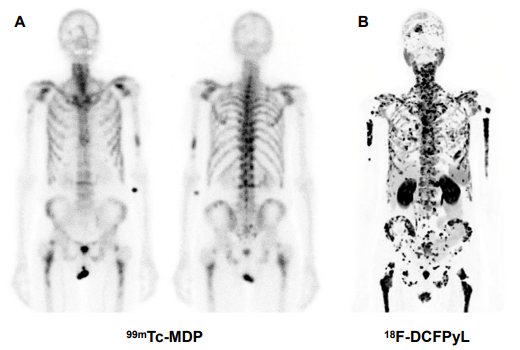
Image Source: Society of Nuclear Medicine and Molecular Imaging
These images were taken of the same patient, one day apart. The images are promising for detecting osseous lesions. Mild uptake is shown on the Tc-MDP bone scan study on the left-hand side compared to the PSMA PET/CT imaging agent on the right hand side. The PSMA PET/CT scan has identified widespread bone metastasis throughout the patient, which will most likely impact the treatment plan and potentially, overall outcome for this patient. This suggests that embracing newer radiopharmaceuticals, imaging procedures, and modalities may help ensure having the best available data for a study.
There are a number of common optional maneuvers that can be incorporated into the PMSA PET/CT imaging. Two of the most common are:
- Use of CT venous contrast during the CT portion of the scan
- Administering furosemide (Lasix) prior to imaging
Since the imaging tracer exits the body through the urinary tract, the bladder tends to fill up with hot or radioactive urine. A common issue that prostate cancer patients might experience is difficulty urinating or emptying the bladder completely, which may obscure any malignant lesions or cells within the pelvic region. By providing furosemide and hydration, the patient is able to expel more radioactive urine and any that does remain within the bladder tends to become diluted or less intense with radiation. This methodology can help provide the reader with a less obstructed view of the pelvic structures.
Highlights from the Q and A
Q I noticed that the two imaging modalities discussed were nuclear based. Are there any other ways that research teams image prostate cancer?
A Historically, some of the traditional ways to image prostate cancer include utilizing a transrectal ultrasound, particularly for biopsy purposes, morphologic T-2 weighted prostate MRIs, and PET/CT and PET/MRI (especially as more facilities gain access to PET machines). In nuclear medicine, bone scans are still very common, such as bone scintigraphy discussed earlier. Some facilities are moving to other, more sensitive, imaging modalities such as the PSMA PET/CT scans discussed above.
There are also some additional assessment methodologies or ways to quantify the bone scans such as a bone scan index. Because the PCWG3 only assesses the bone count or lesion count as the driving factor for determining progressive disease, there have been concerns raised that preexisting bone lesions that light up in the bone scans only have a count as the way to assess them. This doesn’t provide a quantitative measurement methodology for nuclear medicine. PSMA adds a lot of value as possibly using uptake or a volume assessment. The bone scan index is also something that could be added for assessing bone lesions in prostate cancer patients.
Why MERIT?
Medical Expertise. Transparency. Partnership.
MERIT is a global clinical trial imaging endpoint expert providing reliable and attentive expertise in various therapeutic areas, including oncology. MERIT offers:
- High-quality, consistent data review and interpretation by our board-certified clinical trial readers, supported by a team of experienced project managers, data managers, and technologists
- Automation and transparency in a single system for all image and workflow management through EXCELSIOR™, our cloud-based imaging platform
- Scalable solutions and personalized attention from our collaborative, partnership-driven approach
If you’re looking for a partner that will bring dedication and expertise to your clinical trial, consider MERIT.
Click here to see the full webinar
References
Fendler WP, Eiber M, Beheshti M, Bomanji J, Calais J, Ceci F, Cho SY, Fanti S, Giesel FL, Goffin K, Haberkorn U, Jacene H, Koo PJ, Kopka K, Krause BJ, Lindenberg L, Marcus C, Mottaghy FM, Oprea-Lager DE, Osborne JR, Piert M, Rowe SP, Schöder H, Wan S, Wester HJ, Hope TA, Herrmann K. PSMA PET/CT: joint EANM procedure guideline/SNMMI procedure standard for prostate cancer imaging 2.0. Eur J Nucl Med Mol Imaging. 2023 Jan 5. doi: 10.1007/s00259-022-06089-w. Epub ahead of print. PMID: 36604326.
Ozdemir, S., Ersay, A.R., Koc Ozturk, F. et al. Predictive value of standard serum markers for bone metastases in prostate cancer. Afr J Urol 27, 69 (2021). https://doi.org/10.1186/s12301-021-00170-w
https://www.radiologyinfo.org/en/info/bone-scan
https://www.cancer.gov/news-events/cancer-currents-blog/2020/prostate-cancer-psma-pet-ct-metastasis


